Utility of a Family Health History
Introduction
Family health history is an important part of a person's medical record. When visiting a physician for the first time, a patient is often asked in person or on paper, about the health history of themselves and their relatives. This process helps the healthcare provider get to know their patient and provides important information about their health. This information is often collected on a pedigree - a visual representation of family members and their relationships.
The skill of taking and analyzing a minimum of a three-generation family health history is a fundamental skill for all healthcare providers (NCHPEG, 2007). Within this history, the clinician looks for clues that might point to rare hereditary conditions and patients who may benefit from specialized genetic services. The provider also looks at the history through the lens of common complex conditions like diabetes and heart disease, knowing that a family history may indicate an increased risk.
Family Health History in the Clinic
In collecting a family health history, there are some common questions that are asked in nearly every medical situation â gender, current age (or age of death) and major medical diagnoses (with age at diagnosis) of close relatives. Depending on the specific healthcare provider and medical specialty in which they work, there may be more targeted questions asked of a patient. For example, an oncologist may focus on cancer diagnoses in a family while a cardiologist might ask about heart disease, abnormal heart rhythms and sudden deaths.
Genetics specialists (medical geneticists and genetic counselors) are experts in the collection and analysis of a detailed pedigree. They use the patientâs family history and knowledge of inheritance patterns (i.e dominant, recessive, x-linked, etc) to determine individuals in the family who may be at risk for disease. When a genetic diagnosis is suspected, genetic testing is often undertaken to identify the specific genetic change responsible for the disease. If found, this allows a diagnosis to be confirmed and unaffected relatives to be tested to determine whether or not they are at risk for the condition.
Previously the use of genetic information in medical care was confined to medical genetics clinics and the management of single-gene (Mendelian) diseases. Today it is critical for all healthcare professionals to be able to understand and use genetic information in their practice. It is important that primary care providers and non-genetics specialists can identify âred flagsâ of hereditary disease (link out to other page with red flags) in a family health history, and refer patients to genetics specialists for follow-up.
Medical providers should also be on the lookout for family history indications of increased risk for common complex diseases such as type 2 diabetes and heart disease. These conditions are caused by an interaction of multiple environmental and genetic factors, and while there is nothing that can be done to mitigate genetic risk, there are often lifestyle and environment modifications that can be done to help lower overall disease risk.
Case Scenarios
Primary Care
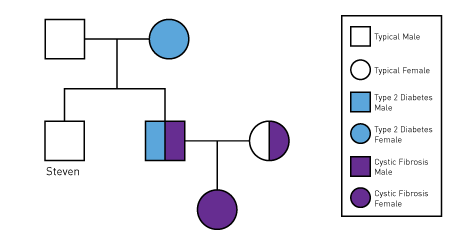
Steven schedules an appointment with his primary care physician for his yearly physical exam. Upon arriving a nurse takes his vital signs and asks Steven whether there have been any changes to his personal or family history over the past year. He recalls that his brother and mother were both recently diagnosed with type 2 diabetes and his 6 month old niece was determined to have cystic fibrosis shortly after birth.
Steven's physician recognizes that having two first-degree relatives with diabetes could indicate an increased risk for Steven. She orders baseline tests to check Steven's glucose tolerance and discusses ways to reduce diabetes risk through lifestyle. In addition, she knows that cystic fibrosis is inherited in a recessive pattern and that Steven may be a carrier for the condition. While it would not impact his medical care, determining whether he is a CF carrier could impact his, and his children's, decisions on reproduction and prenatal testing. Steven's physician refers him to a local genetics specialist to discuss CF and carrier testing in more detail.
Specialty Clinic
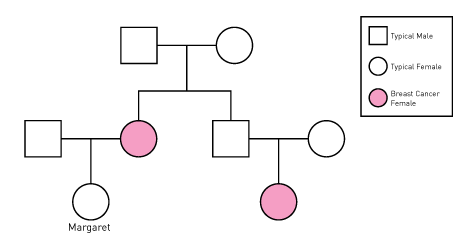
Margaret is diligent in having yearly breast cancer screenings. She knows a lot about breast cancer since her mother was diagnosed with it at 60 and her maternal cousin was recently diagnosed at age 57. At her annual mammogram appointment she discusses her family history with the physician and asks what her personal risk for breast cancer might be. The physician does not see evidence of a rare hereditary form of cancer susceptibility in Margaret's family history, but does acknowledge that having a family history of breast cancer may impact her risk. He runs a computerized risk model that takes into account family history as well as her past medical history that indicates a lifetime breast cancer risk of ~18%, mildly increased from the general population lifetime risk of ~12%. The doctor instructs Margaret to remain diligent with screenings and take steps to reduce her environmental risk factors such as maintaining a healthy weight and not drinking excessive amount of alcohol.
Medical Genetics
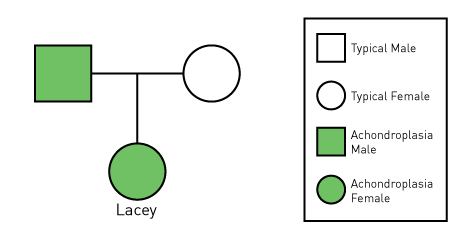
Lacey has been followed by a medical geneticist since birth, when she was diagnosed with achondroplasia (the most common form of dwarfism). Her family was not surprised at the diagnosis, since her father also has short stature. Achondroplasia is a Mendelian condition inherited in a dominant fashion, meaning Lacey's father has a 50% chance of passing on the condition with each pregnancy. Likewise, any children Lacey may have in the future would have this same 50% chance of being affected (assuming her partner is unaffected). Almost all cases of achondroplasia are caused by a single DNA letter change (mutation) in the FGFR3 gene. Lacey had genetic testing for this specific genetic change as a baby to confirm the cause of her short stature. There is no other family history of the condition, so the FGFR3 mutation leading to achondroplasia in Lacey's family likely occurred in the family for the first time in Lacey's father. Lacey will be followed by genetics annually to make sure she is getting appropriate medical care and to address any questions or concerns that come up.